Medical needles are among the most widely used medical devices in modern healthcare, supporting applications that range from routine vaccination to complex diagnostic and interventional procedures. Despite their apparent simplicity, needles are highly engineered products whose performance depends on precise control of gauge, length, bevel geometry, material properties, and safety mechanisms.
Globally, billions of injections and needle-based procedures are performed each year. As a result, improper needle selection or suboptimal design can have far-reaching consequences, including inaccurate drug delivery, increased patient discomfort, tissue injury, diagnostic error, and occupational exposure to bloodborne pathogens.
This article provides a structured, technical overview of the principal types of medical needles used worldwide. It is intended for healthcare professionals, clinical procurement teams, and device specialists who require a clear understanding of needle classification, design rationale, and clinical application.
Overview of Major Medical Needle Categories and Clinical Applications:
| Needle Category | Primary Clinical Use | Typical Users | Key Design Objective |
|---|---|---|---|
| Hypodermic needles | Drug injection | Nurses, physicians | Accurate delivery to target tissue |
| Insulin needles | Diabetes management | Patients, nurses | Minimal pain, dosing precision |
| IV catheter needles | Venous access | Nurses, clinicians | Secure vascular access |
| Butterfly needles | Venipuncture, short infusion | Phlebotomists, nurses | Control and vein protection |
| Blood collection needles | Diagnostic sampling | Phlebotomists | Consistent blood flow, safety |
| Spinal needles | Spinal anesthesia, CSF sampling | Anesthesiologists | Atraumatic dural access |
| Epidural needles | Epidural anesthesia | Anesthesiologists | Catheter placement accuracy |
| Huber needles | Implanted port access | Oncology nurses | Non-coring septum access |
| Aspiration needles | Cytology, fluid removal | Radiologists, surgeons | Minimal tissue trauma |
| Core biopsy needles | Histological diagnosis | Radiologists, surgeons | Intact tissue sampling |
| Surgical suture needles | Tissue closure | Surgeons | Tissue preservation |
| Filter / blunt fill needles | Medication preparation | Pharmacists, nurses | Accurate delivery to the target tissue |
1. Hypodermic Needles
Hypodermic needles are hollow, sharp cannulas designed to penetrate the skin and deliver or withdraw fluids. They are typically classified by gauge (G), which indicates outer diameter, and longueur, which determines penetration depth. The bevel angle, wall thickness, and surface lubrication also influence the insertion force and flow characteristics.
Hypodermic needles are generally subdivided according to the target tissue layer.
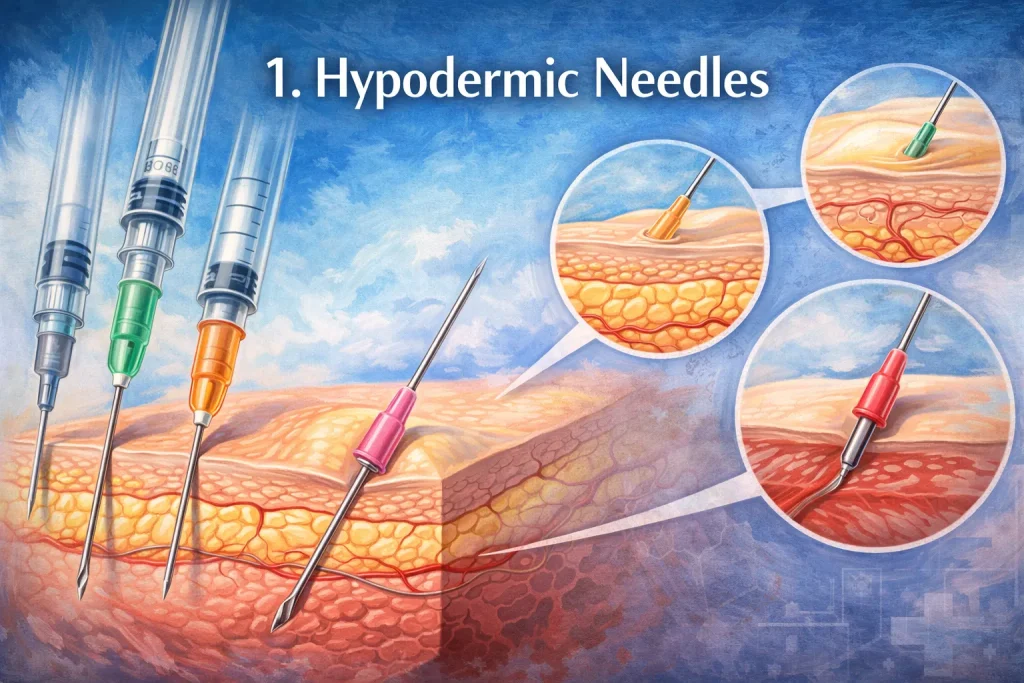
1.1 Intradermal Injection Needles
Intradermal needles are designed for extremely shallow injections into the dermis. Because this layer has limited vascularity, intradermal delivery is primarily used for diagnostic and immunologic testing rather than systemic therapy.
Key characteristics include short length, fine gauge, and precise bevel geometry to allow controlled wheal formation.
1.2 Subcutaneous Injection Needles
Subcutaneous needles penetrate the fatty tissue beneath the skin and are commonly used for medications that require slow, sustained absorption. These needles balance minimal patient discomfort with sufficient rigidity for reliable insertion.
Subcutaneous injection is commonly used for insulin, anticoagulants, hormones, and selected vaccines.
1.3 Intramuscular Injection Needles
Intramuscular needles are longer and typically of lower gauge than intradermal or subcutaneous needles. They are designed to traverse skin and adipose tissue to reach skeletal muscle, enabling faster absorption and larger injection volumes.
Hypodermic Needle Types by Injection Depth:
| Injection Type | Target Tissue | Calibre typique (G) | Typical Length | Common Applications |
|---|---|---|---|---|
| Intradermal (ID) | Dermis | 25–27 G | 6–13 mm | TB tests, allergy tests |
| Subcutaneous (SC) | Subcutaneous fat | 25–30 G | 8–16 mm | Insulin, anticoagulants |
| Intramuscular (IM) | Skeletal muscle | 20–25 G | 25–38 mm | Vaccines, antibiotics |
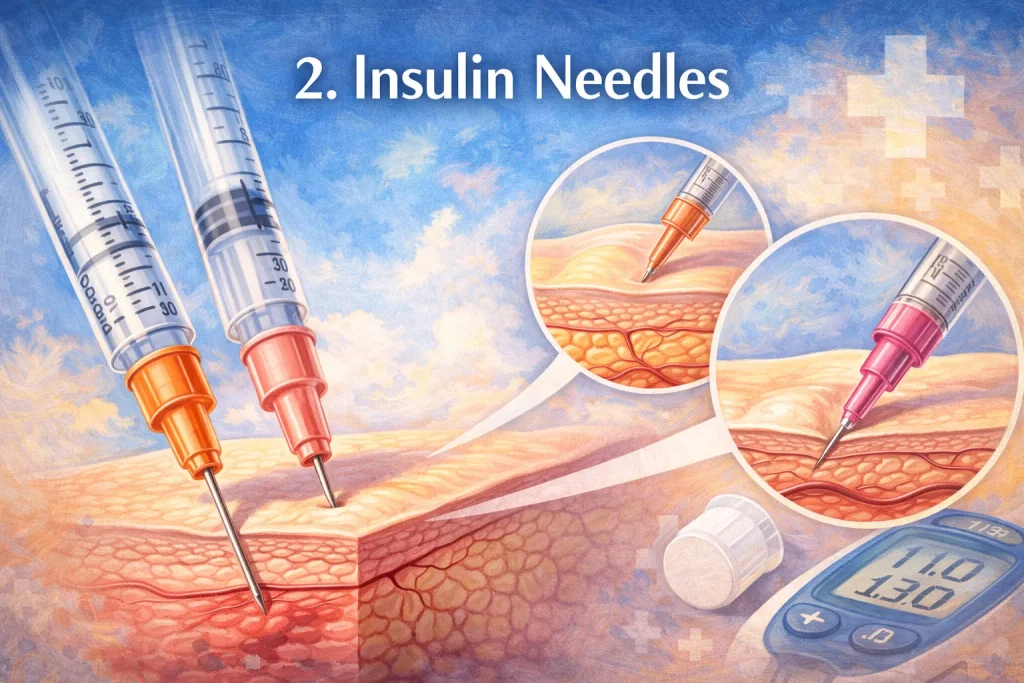
2. Insulin Needles
Insulin needles represent a specialized category of hypodermic needles optimized for frequent, self-administered injections. Their design prioritizes patient comfort, dosing accuracy, and consistency across a wide range of body types.
These needles are typically ultra-fine in gauge and very short in length, significantly reducing insertion pain and minimizing the risk of accidental intramuscular injection. Most insulin needles are permanently attached to insulin syringes to reduce dead space and dosing variability.
Comparison of Insulin Needles vs Standard Subcutaneous Needles:
| Paramètres | Insulin Needles | Standard SC Needles |
|---|---|---|
| Typical gauge | 29–32 G | 25–27 G |
| Typical length | 4–12 mm | 8–16 mm |
| Injection frequency | Multiple times daily | Occasional |
| Syringe integration | Usually fixed | Often detachable |
| Pain optimization | Very high | Moderate |
| Risk of IM injection | Very low | Higher in thin patients |
3. Intravenous and Venous Access Needles
3.1 IV Catheter Needles
IV catheter needles are used to introduce flexible catheters into peripheral veins. After venous access is established, the steel needle is withdrawn while the catheter remains in place, allowing continuous or intermittent infusion.
Gauge selection depends on clinical context, required flow rate, and patient anatomy. Larger gauges support rapid infusion, while smaller gauges are preferred for pediatric or fragile veins.
3.2 Butterfly (Winged Infusion) Needles
Butterfly needles consist of a short steel needle, flexible wings, and extension tubing. Their design allows shallow insertion angles and improved control, making them particularly useful for venipuncture and short-duration infusions.
Butterfly needles are frequently used in pediatrics, geriatrics, and patients with difficult venous access.
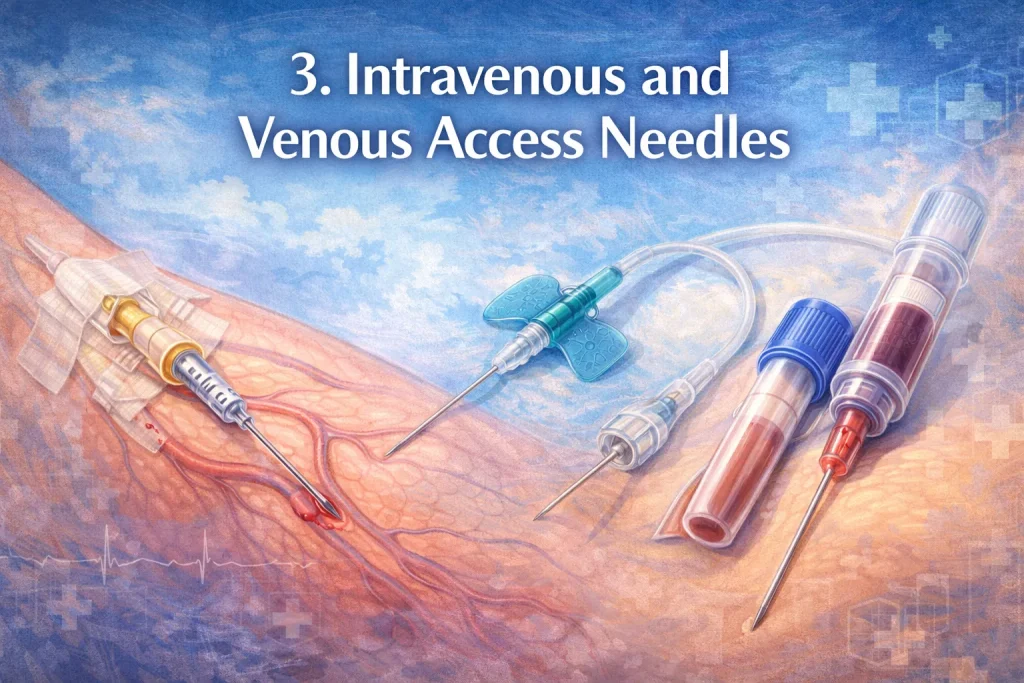
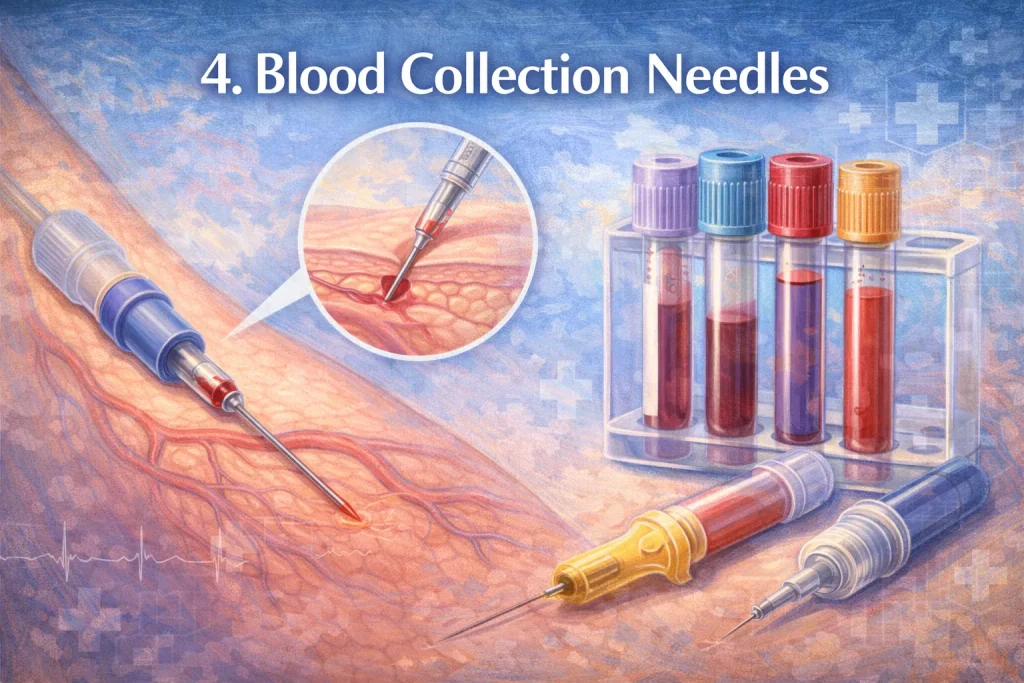
4. Blood Collection Needles
Blood collection needles are specifically engineered for phlebotomy and diagnostic sampling rather than medication delivery. They are commonly used with evacuated tube systems and are designed to provide consistent blood flow while minimizing hemolysis.
Modern blood collection needles almost universally incorporate safety mechanisms to reduce the risk of needlestick injuries in high-throughput laboratory environments.
Intravenous Access Devices Comparison:
| Device Type | Typical Gauge | Duration of Use | Flow Capacity | Typical Indications |
|---|---|---|---|---|
| IV catheter needle | 14–24 G | Hours to days | High | Continuous infusion |
| Butterfly needle | 18–27 G | Minutes to hours | Low–moderate | Venipuncture, pediatrics |
| Blood collection needle | 21–23 G | Single use | Moderate | Diagnostic blood draw |
5. Anesthesia and Specialized Access Needles
5.1 Spinal Needles
Spinal needles are used for lumbar puncture and spinal anesthesia. Contemporary designs increasingly favor atraumatic, pencil-point tips, which separate rather than cut dural fibers, reducing the incidence of post-dural puncture headache.
5.2 Epidural Needles
Epidural needles are larger and structurally distinct from spinal needles. The curved Tuohy tip facilitates catheter advancement into the epidural space while minimizing the risk of dural puncture.
5.3 Huber Needles
Huber needles are non-coring needles designed specifically for accessing implanted vascular ports. Their angled tip prevents coring of the silicone septum, preserving port integrity and extending device lifespan.
Anesthesia and Specialized Access Needles:
| Type d'aiguille | Typical Gauge | Conception de l'embout | Primary Function |
|---|---|---|---|
| Spinal needle (pencil-point) | 22-27 G | Atraumatic, rounded | Spinal anesthesia, CSF sampling |
| Spinal needle (cutting) | 22–25 G | Cutting bevel | Diagnostic lumbar puncture |
| Epidural (Tuohy) needle | 16-18 G | Curved, blunt | Epidural catheter placement |
| Huber needle | 19–22 G | Angled, non-coring | Implanted port access |

6. Biopsy and Aspiration Needles
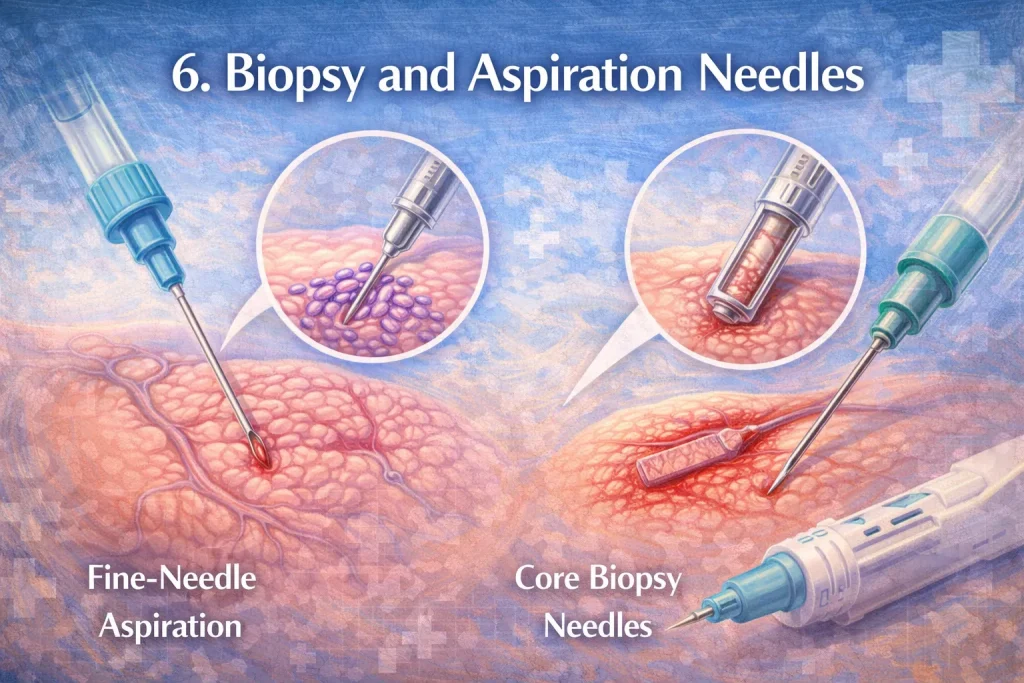
6.1 Aspiration Needles
Aspiration needles are long, fine-gauge needles used to withdraw cells or fluids for cytological analysis. Their design minimizes tissue disruption while allowing adequate sample acquisition.
They are commonly used in fine-needle aspiration procedures involving the thyroid, lymph nodes, breast, and soft tissue masses.
6.2 Core Biopsy Needles
Core biopsy needles are designed to remove intact cylindrical tissue samples suitable for histopathological examination. They are typically larger in gauge and may be used manually or with automated biopsy systems.
Biopsy and Aspiration Needle Comparison:
| Fonctionnalité | Aspiration Needles (FNA) | Core Biopsy Needles |
|---|---|---|
| Typical gauge | 22–25 G | 14-18 G |
| Sample type | Cells, fluid | Solid tissue core |
| Tissue trauma | Minimal | Moderate |
| Diagnostic use | Cytology | Histopathology |
| Common specialties | Endocrinology, radiology | Oncology, radiology |
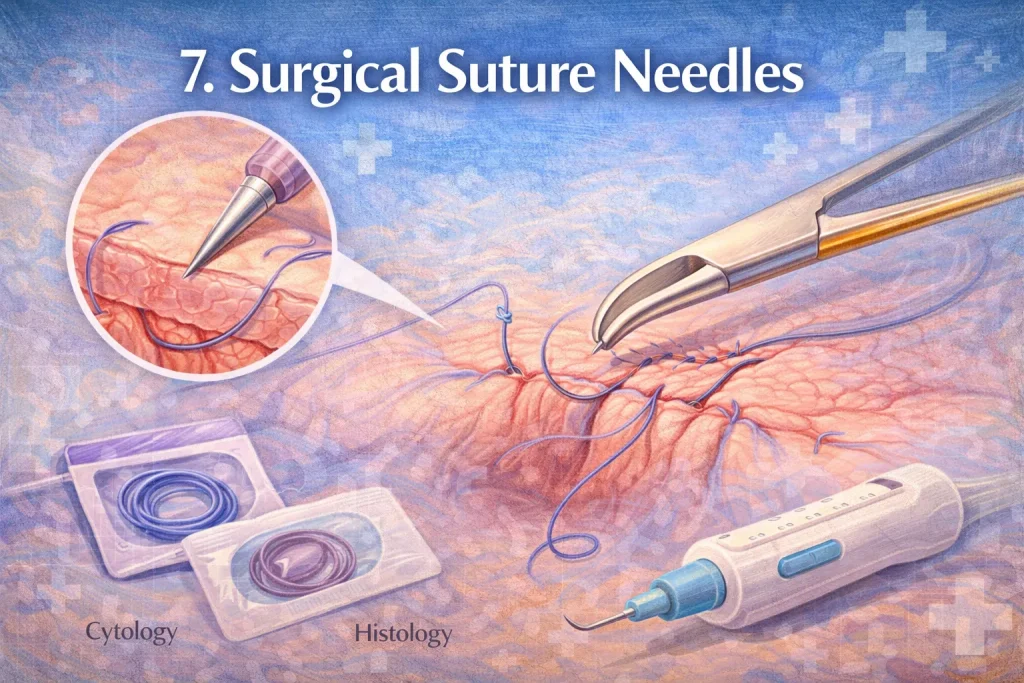
7. Surgical Suture Needles
Surgical suture needles differ fundamentally from injection needles. Taper-point suture needles have a round cross-section that dilates tissue rather than cutting it, making them suitable for soft tissue closure where minimizing trauma is critical.
These needles are commonly used in muscle, fascia, and visceral surgery.
Surgical and Medication Preparation Needles:
| Type d'aiguille | Tip Geometry | Primary Use | Safety Advantage |
|---|---|---|---|
| Taper-point suture needle | Round, non-cutting | Soft tissue closure | Reduced tissue tearing |
| Filter needle | Blunt with microfilter | Ampoule medication withdrawal | Particle filtration |
| Blunt fill needle | Fully blunt | Vial access, drug prep | Blunt with a microfilter |
8. Medication Preparation Needles
8.1 Filter Needles
Filter needles incorporate an integrated microfilter, typically 5 microns, to remove particulate contamination when withdrawing medication from glass ampoules. They are intended solely for medication preparation and must be replaced before administration.
8.2 Blunt Fill Needles
Blunt fill needles are non-sharp needles used for vial access and medication preparation. Their inability to penetrate skin significantly reduces the risk of accidental needlestick injury while maintaining adequate flow performance.
9. Safety Needles and Regulatory Considerations
Safety-engineered needles are designed to reduce occupational exposure to bloodborne pathogens. These devices incorporate features such as sliding shields, automatic retraction, or blunt technology to cover or eliminate the sharp tip after use.
Regulatory bodies worldwide increasingly mandate or recommend the use of safety needles, particularly in high-risk settings such as phlebotomy, vaccination campaigns, and hospital wards.
Safety Needle Technologies and Mechanisms:
| Safety Mechanism | Activation Type | Typical Applications | Injury Reduction Benefit |
|---|---|---|---|
| Sliding shield | Manual or passive | Hypodermic, phlebotomy | Immediate tip coverage |
| Retractable needle | Automatic | Syringes, IV access | Complete needle removal |
| Blunt technology | Passive | Medication prep | Prevents skin penetration |
| Needleless systems | Passive | IV connectors | Eliminates sharps entirely |
Conclusion
Medical needles are precision devices whose design and application directly influence clinical outcomes, patient experience, and healthcare worker safety. Understanding the distinctions among needle types is essential for proper clinical use, informed procurement, and regulatory compliance.
As global standards evolve and safety expectations increase, continued innovation and education in needle technology remain critical to advancing patient care and occupational health.
FAQ
Lower gauge needles have larger diameters, allowing higher flow but potentially more discomfort. Higher gauge needles reduce pain but limit flow.
Shorter lengths reduce the risk of accidental intramuscular injection and improve consistency across patient body types.
Butterfly needles are preferred for short procedures, fragile veins, or pediatric patients, while IV catheters are better for ongoing infusions.
Their non-coring tip preserves the integrity of the port septum, extending device lifespan and preventing leakage.
While not universally mandatory, they are strongly recommended to prevent glass particle contamination.
They incorporate shielding or retraction mechanisms that cover the needle immediately after use, minimizing accidental exposure.